Questions about weight loss injections for insulin resistance are becoming more common, particularly among people who find that traditional weight loss advice has had limited effect.
Online discussions often blur the lines between insulin resistance, diabetes, and injectable treatments, which can make it difficult to understand what these medications are actually used for.
This article looks at how insulin resistance can influence weight, why weight loss may feel more difficult in this context, and how weight loss injections are sometimes discussed as part of medical care. The aim is to clarify common areas of confusion and set realistic expectations, focusing on understanding rather than outcomes or guarantees.
Understanding Insulin Resistance and Its Impact on Weight
Insulin resistance occurs when the body becomes less responsive to insulin, a hormone involved in regulating blood sugar and energy storage.
As a result, the body may produce higher levels of insulin to compensate, which can influence appetite, energy use, and how fat is stored.
For many people, insulin resistance does not cause obvious symptoms. Instead, it may appear as difficulty losing weight, increased hunger, or feeling fatigued despite consistent lifestyle efforts. This can make weight loss feel unpredictable or disproportionately challenging.
Because insulin resistance alters how the body handles energy, weight changes may not follow the same patterns seen in people without underlying metabolic disruption. This is one reason weight loss injections for insulin resistance are sometimes discussed, although their role is often misunderstood.
Importantly, insulin resistance exists on a spectrum and is not the same as type 2 diabetes, which is why treatment decisions are typically based on overall metabolic context rather than weight alone.
Why Insulin Resistance Can Make Weight Loss Less Predictable?
Once insulin resistance is present, weight loss efforts may not produce the same results seen in people without underlying insulin sensitivity issues.
Insulin plays a role not only in blood sugar regulation but also in how energy is stored and released. When cells respond less effectively to insulin, the body may compensate by producing more of it, which can influence hunger signals and fat storage.
For many people, this means that reducing calorie intake does not always lead to predictable weight loss. Appetite may feel harder to regulate, energy levels may fluctuate, and weight changes can seem slower or inconsistent despite sustained effort.
This experience is often described by people exploring insulin resistance weight loss, particularly when conventional advice has not produced expected results.
Understanding this context is important before considering treatment options. It helps explain why weight management strategies are sometimes adjusted when insulin resistance is part of the picture, and why expectations around progress often need to be more individualised rather than outcome-driven.
What Is Meant by “Weight Loss Injections” in Medical Care
The phrase weight loss injections is commonly used in online searches, but it is rarely defined clearly. In most cases, it refers to prescription medications that influence appetite regulation and satiety through hormonal pathways, rather than injections of insulin itself.
These treatments are often discussed together because they are injectable and used within medical weight management, even though they are not interchangeable. Medications such as Mounjaro, Ozempic, and Wegovy are examples that are frequently mentioned in this context.
Importantly, weight loss injections do not act independently of the body.
They modify appetite-related signalling, which means their effects depend on individual physiology, tolerance, and how the treatment is used over time. This variability is one reason broad claims about outcomes or suitability can be misleading, particularly when insulin resistance is involved.
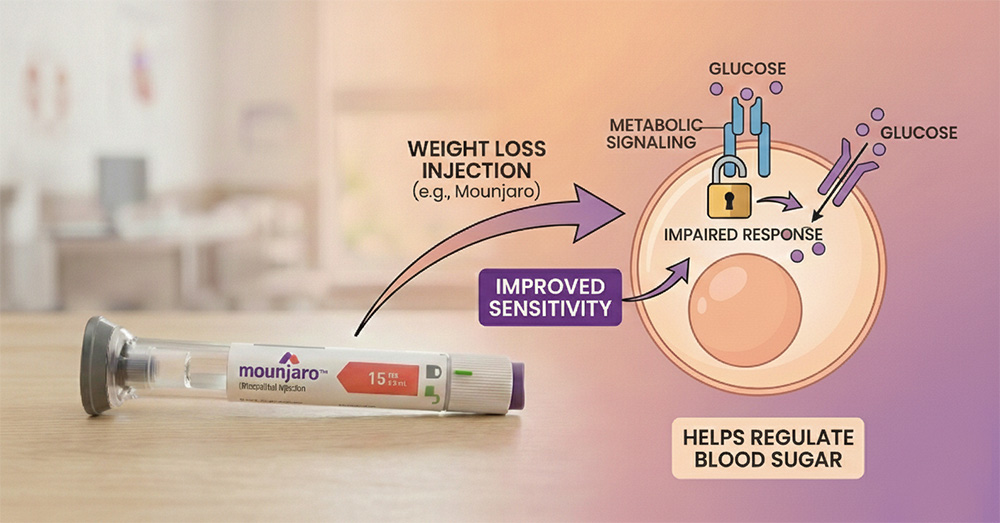
How Weight Loss Injections May Influence Insulin Sensitivity
Once insulin resistance is present, weight loss injections are often discussed in relation to insulin sensitivity, not just weight change alone.
GLP-1–based medications primarily support appetite regulation and weight reduction, but research also shows they can have direct effects on insulin sensitivity through multiple biological mechanisms.
In addition to reducing body weight, these medications have been shown to influence glucose handling, inflammation, and lipid metabolism in insulin-dependent tissues. In some individuals, improvements in insulin sensitivity are therefore not solely attributable to weight loss, although the degree of metabolic response varies between patients.
It’s also important to recognise that medication does not act in isolation. The body responds based on existing metabolic health, lifestyle factors, and overall physiology. For this reason, weight loss injections are typically considered as part of a broader medical approach rather than as a targeted solution for insulin resistance itself.
Who Is Suitable for Weight Loss Injections?
Not everyone with insulin resistance is automatically considered suitable for weight loss injections. Decisions around use are usually guided by overall health context rather than weight alone.
Medical assessment often considers factors such as existing metabolic conditions, medication history, and potential contraindications. This screening process helps identify who may benefit, who may require closer monitoring, and who should avoid treatment altogether.
Weight loss injections such as Mounjaro, Ozempic, and Wegovy are often discussed together, but they are not interchangeable and are not appropriate for every individual.
This is why eligibility screening is a central part of responsible care, particularly when insulin resistance is present. Treatment decisions are typically individualised, based on risk–benefit considerations rather than assumptions about effectiveness.
Clearing Up Common Confusion Around Injections and Insulin
People researching weight loss injections for insulin resistance often encounter overlapping or misleading information. The points below address the most common areas of confusion clearly and directly.
Weight loss injections are not the same as insulin.
Weight loss injections are prescription medications that influence appetite and satiety. They are not insulin replacement therapy and do not supply insulin to the body.
How Weight Loss Injections Affect Blood Sugar Regulation
Weight loss injections are not insulin replacement therapy, but many GLP-1–based medications do have direct effects on blood sugar regulation. They help lower blood glucose by stimulating insulin release, reducing glucagon secretion, and slowing gastric emptying, in addition to supporting appetite regulation and weight loss.
Weight loss injections differ from insulin injections used in diabetes care.
Insulin injections are prescribed when the body cannot produce or use insulin effectively. Weight loss injections act on appetite-related pathways and serve a different medical purpose.
Weight loss injections are not universally suitable for everyone, and treatment decisions are individualised.
Medications such as Mounjaro, Ozempic, and Wegovy may be changed or adjusted over time under medical supervision, depending on response, tolerance, and individual health factors rather than medication name alone.
What to Expect When Weight Loss Injections Are Used in Insulin Resistance
When weight loss injections are used in the context of insulin resistance, experiences vary. Some people notice changes in appetite or eating patterns, while others observe more gradual or subtle effects. Side effects and tolerance also differ between individuals.
What matters most is that these treatments are approached as part of a broader medical plan rather than a stand-alone solution. There are no fixed timelines, no guaranteed outcomes, and no single pattern that applies to everyone. This variability is why expectations are typically shaped through monitoring and review rather than assumptions.
Conclusion
Interest in weight loss injections for insulin resistance reflects a broader need for clearer, more realistic discussions around metabolic health and weight management. Insulin resistance can affect how the body responds to weight loss efforts, which is why treatment decisions are usually individualised. Weight loss injections may be considered in some cases, but they are not universal solutions or substitutes for medical assessment. Understanding the distinctions between insulin resistance, injectable treatments, and individual variability allows for more informed and grounded decision-making.
Frequently Asked Questions
Do weight loss injections treat insulin resistance directly?
Weight loss injections do not directly treat insulin resistance. They influence appetite and eating behaviour, and any metabolic changes usually occur indirectly alongside weight or lifestyle changes rather than through a targeted insulin-sensitising effect.
Are weight loss injections the same as insulin injections?
No. Insulin injections are prescribed to manage blood sugar when insulin production or use is impaired. Weight loss injections act on appetite-related pathways and are not a form of insulin therapy.
Can people with insulin resistance use weight loss injections?
Some individuals with insulin resistance may be considered after medical assessment, while others may not. Clinics such as Endocare focus on suitability, safety, and overall health context rather than assuming these treatments are appropriate for everyone.
Should weight loss injections be used without medical guidance?
No. These are prescription treatments that require assessment and monitoring. At Endocare, decisions around weight loss injections are guided by individual metabolic factors rather than trends or online claims.